The IMCAN study:
Improving Muslim Women CANcer Screening Uptake
The word ‘imkān’ (إمكان) in Arabic means possibility, opportunity or capability and that’s exactly what this project is about.
The IMCAN study, funded by Cancer Research UK, focuses on improving participation in breast, cervical and bowel screening among Muslim women in the UK.
We know that some women face unique barriers to screening, and that these can lead to later diagnoses and poorer health outcomes.
In 2021, working closely with Muslim women in the North East of England and Scotland, we co-designed an intervention to support informed decision-making and increase engagement with screening.
The IMCAN study is focused on testing whether this intervention is feasible and acceptable. This is research done with the community, for the community. It is rooted in the belief that everyone should have the opportunity (imkān) for good health, early diagnosis and better outcomes.
IMCAN study duration: January 2023–June 2026
Why this study matters
Breast cancer is the most common cancer in women in the UK.
Around 1 in 7 women will be diagnosed with it during their lifetime.
The risk of bowel and cervical cancer is also important: 1 in 18 women may get bowel cancer, and 1 in 142 women may get cervical cancer.*
If these cancers are not found early, treatment can be harder, more painful, and may take longer. Sadly, this can also lead to more people dying. But when cancer is found early, treatment often works better and more lives can be saved. That’s why going to your cancer screening appointments is so important.
*Based on Cancer Research UK data
The NHS runs national screening programmes for breast, bowel, and cervical cancer.
Women who are eligible will get an invitation in the post when it's time for them to be screened. However, not everyone goes to their screening when invited.
In the UK, in 2021/22, the number of people who took part in screening was:
Around 62-70% for bowel cancer
62-77% for breast cancer
67-69% for cervical cancer
Among women from ethnic minority backgrounds, screening rates are even lower.
This means some may be diagnosed later, when cancer is harder to treat.
Muslim women make up about one-third of the UK’s ethnic minority population. This means they may be more affected by the impact of late diagnosis.
Reasons why Muslim women might not go for screening
In our earlier research, Muslim women shared some of the reasons why they might not go for screening. These included:
not knowing about screening
feeling embarrassed
being worried about seeing a male doctor
finding bowel cancer screening too disgusting
To help improve cancer screening uptake among Muslim women, we recognised that general public health messages may not always work for everyone. Muslim women may have different concerns or experiences that are not addressed in mainstream campaigns. So, we designed this project using three key principles:
Tailored messages
We used health messages that are respectful of and consistent with Muslim women’s beliefs.Community partnership
We worked closely with members of the Muslim community to guide the project and ensure it was relevant and respectful.Peer facilitators
We trained Muslim women from the community to deliver the workshop, so that messages would come from trusted voices within the community.
Before we started the IMCAN study, we did a pilot study in which we developed the workshop tested in IMCAN.
During 2020–2021, funded by the Scottish Government’s Inequalities Fund, we worked with 10 Muslim women in Scotland to design a workshop that aims to improve cancer screening uptake.
The final workshop includes four key parts:
A peer-led discussion about what makes it harder or easier to go for screening
A health education session with clear and simple information
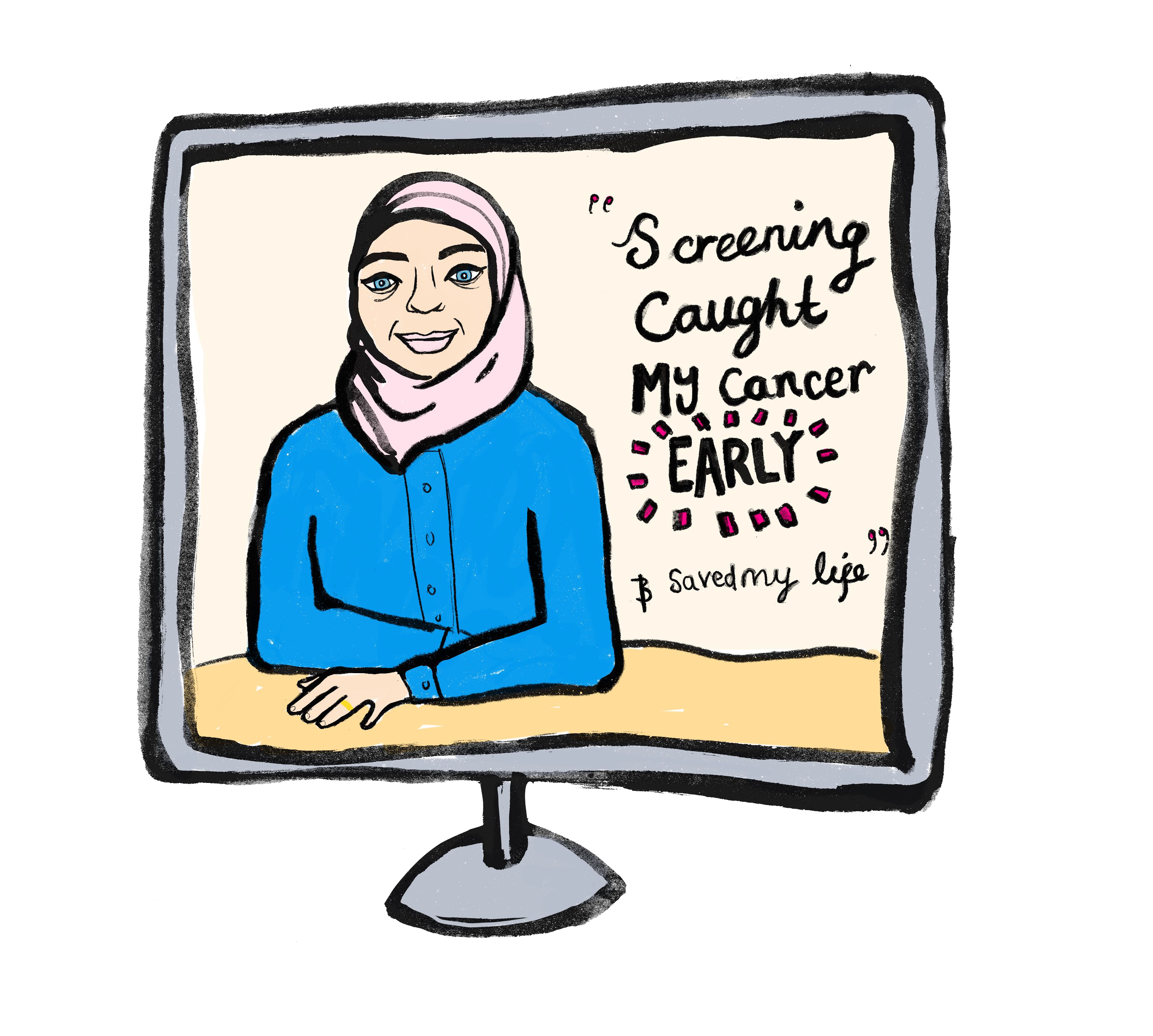
Videos of Muslim women sharing their own experiences of cancer screening
A faith-based message that explains cancer screening from an Islamic perspective
The pilot before the IMCAN study
Part 1:
Barriers and Enablers
A peer-led discussion of barrier and enablers to breast, bowel and cervical cancer screening
Part 2:
Health Education
A health education session led by a female GP on screening followed by Q&A
Part 3:
Testimonials
Videos of Muslim women’s experiences of cancer or screening
Part 4:
Faith as Enabler
A religious perspective on cancer screening delivered by a female religious scholar
The co-designed workshop mixes general health education messages on cancer screening along with a faith component. Here, faith is an enabler for screening; the messages for this part of the workshop were developed and delivered by a female religious scholar (Alimah). Read more information about this study in this blog or this academic paper.
The workshop was delivered online in 2021 with 18 Scottish Muslim women of Arabic and Asian ethnicities. The workshop participants then took part in focus groups one week after the workshop; they described the content of the workshop and methods of delivery to be highly acceptable.
Building on the pilot:
the IMCAN study
Following the pilot study, we obtained funding from Cancer Research UK for the IMCAN study to investigate whether we could run a trial to test how effective our faith-based workshop is at improving the uptake of breast, bowel and cervical cancer screening. The IMCAN study started on the 1st of January 2023 and will complete on the 30th of June 2026. We have four parts to the study that we call ‘work packages’.
Part 1:
Delivering the workshop
We recruited 261 Muslim women to take part in our co-designed cancer screening workshop, either online or in person. The workshops were delivered by trained peer educators from the Muslim community.
Participants completed questionnaires before the workshop, and again at 6 months and 12 months afterwards, to assess changes in their knowledge, attitudes, and intentions to attend cancer screening. We also look at whether participants attend screening during this time.
Part 2:
Understanding experiences
After the workshops, we invited some participants for a focus group or interview to talk about their experiences and how they felt about the workshop. We also interviewed:
stakeholders who helped with recruitment and delivery
peer educators who ran the workshops
These conversations help us understand what worked well, what could be improved, and how to make the intervention even more effective and accessible.
Part 3:
Assessing feasibility
To decide whether it would be possible to run this workshop in a larger randomised controlled trial in the future, we track everything we do:
time and resources needed
number of people involved
costs
training and delivery processes
recruitment progress and any challenges
This will help us understand the practical steps needed for larger-scale implementation.
Part 4:
Sharing what we learn
We will ask participants, peer educators, and stakeholders how we should share the results of the study. This will help us make sure the findings reach the Muslim community, the wider public, and health professionals and policymakers working in cancer screening.
What did we find?
Women said the workshop changed how they felt about screening.
Having an Alimah and a GP speaking in the workshops together was important since women could trust the information they explained.
Women enjoyed the relaxed atmosphere in the workshop, use of clear and simple language, and the chance to ask questions.
Women’s knowledge about cancer and screening more than doubled.
After the workshop, 90% of women said they would attend breast screening, 86% bowel screening, and 82% cervical screening, the next time they were invited.
More women started attending cancer screening.
Woman also changed some of their negative beliefs about screening.
You can download a two-page file with our findings here
You can view the one-minute animation in Urdu here
You can view the one-minute animation in Bengali here
These early results are promising and suggest that the workshop may change how women feel about screening. The next step is to test the workshop with a larger group to find out if it really helps more Muslim women go for screening. This is called a trial.
At the end of our study, we will conclude whether we can run a trial to test if our workshop is effective at increasing breast, bowel and cervical cancer screening uptake among Muslim women.
We hope that the outcomes of our study will guide interventions to tackle cancer screening inequities for Muslim women in the UK and worldwide.
What’s next?

Manual: coming soon
We are developing a manual outlining the steps we took to deliver the IMCAN study. This resource may support other researchers considering similar participatory approaches. We will publish the manual here shortly.
IMCAN team
Project lead
Associate Professor in Public Health for Medicine, School of Medicine, University of Sunderland, UK
Co-lead
Professor of Behavioural Science and Health, School of Health and Wellbeing, University of Glasgow, UK
Mrs Cerysh Sadiq
Community Recruitment Lead and Alimah, School of Medicine, University of Sunderland, UK
Mrs Fozia Haider
Community Recruitment Lead, School of Medicine, University of Sunderland, UK
Research Associate /
Post-doctoral Researcher, School of Medicine, University of Sunderland, UK
Lecturer in Health Psychology/Behavioural Sciences related to Dentistry, Dental School, University of Glasgow, UK
Professor and Vice Chair for Research and Scholarship, Medical College in Wisconsin, USA
Director of Biostatistics, Professor of Clinical Trial Biostatistics, Robertson Centre for Biostatistics, University of Glasgow, UK
GP University Lecturer, School of Health and Wellbeing, University of Glasgow, UK
Senior Lecturer, School of Nursing, University of Sunderland, UK